Searching for the proverbial needle in a haystack. Biomarkers unleashed.
In recent history a phenomenal amount of research, publications and companies have emerged from the worlds of genomics and epigenetics, with a key focus on identifying the reasons why patients present with disease and to identify the traits which might enable us to both diagnose and provide effective treatments.
However, in the majority of diseases there is still a distinct lack of effective ways to qualify patients and quantitate response. For example, in the USA there are at least 8 clinically approved chemotherapeutic interventions for colorectal cancer, and yet no biomarker driven diagnostic which can inform clinicians which intervention is most suitable for their patient.
For immuno-oncology, the situation is even more complex. Only 20-40% of cancer patients could potentially benefit from immunotherapy, but even fewer will have long term disease remission1-3.
Developing a means of identifying groups of patients who will benefit from these agents is critical and requires an improved understanding of the mechanisms of action as well as both primary and acquired resistance, both of which are common yet poorly understood. The risks of toxicities with these agents must also be considered as well as the importance of ensuring that patients are not exposed to ineffective therapies when other active treatments might be available. Even if patients are diagnosed as potential responders to checkpoint inhibitors where PD-L1 expression is used to gate potential responders, response varies tremendously dependent on treatment setting, PD-L1 positivity threshold, diagnostic chosen. Objective response rate can be as low as 14% 4.
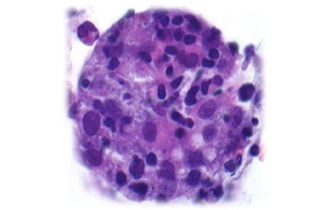
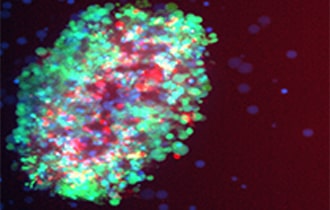
Perhaps the analogy of “searching for a needle in a haystack” is not appropriate. The anatomy of response is clearly complex, multidimensional and interdependent. At Nilogen, we’ve been able to demonstrate in fresh patient tumor tissue that responsiveness to Pembrolizumab is not identified solely by whether a tumor is hot or cold immunologically, nor PD-1 occupancy by Pembrolizumab, but a more subtle collection of multiple readouts including gene expression and cytokine expression, the ratio of M1/M2 macrophages, and their balance with T regs, MDSCs and stromal elements, as well as the expression of innate resistance mechanisms 5,6.
So perhaps, improving the way we develop better drugs, combinations, diagnostics and ultimately treatment is to unleash the potential of functionally characterizing patients in the clinical setting rather than trying to squeeze everyone into one box or another. The financial and human cost of multiple failed interventions is far higher than the cost of an effective multidimensional biomarker strategy.
1. Garon, E. B. et al. Five-year overall survival for patients with advanced non–small-cell lung cancer treated with pembrolizumab: results from the phase I KEYNOTE-001 study. J. Clin. Oncol. 37, 2518–2527 (2019).
2. Brahmer, J. R. et al. The society for immunotherapy of cancer consensus statement on immunotherapy for the treatment of non-small cell lung cancer (NSCLC). J. Immunother. Cancer 6, 75 (2018).
3. Hamid, O. et al. Five-year survival outcomes for patients with advanced melanoma treated with pembrolizumab in KEYNOTE-001. Ann. Oncol. 30, 582–588 (2019).
4. Doroshow, D.B., Bhalla, S., Beasley, M.B. et al. PD-L1 as a biomarker of response to immune-checkpoint inhibitors. Nat Rev Clin Oncol (2021). https://doi.org/10.1038/s41571-021-00473-5
5. Page MM, Mediavilla-Varela M, Kreahling J, Altiok S. P67: Innovative combinatorial approach to characterize the immune landscape and analyze the tumor response after anti-PD-1 blockade in a 3D ex vivo tumoroid system of non-small cell lung cancer. 33rd Annual Meeting & Pre-Conference Programs of the Society for Immunotherapy of Cancer (SITC 2018); Washington, D.C., USA. 7-11 November 2018. Journal for ImmunoTherapy of Cancer. 2018; 6(Suppl 1):114. DOI: 10.1186/s40425-018-0422-y
6. Agrawal V, Pabon MM, Pastoor T, Kreahling J, Altiok S. P740: Leveraging Artificial Intelligence to Advance Immuno-oncology Drug Development Using Functional Ex Vivo 3D-tumor Organoid Platforms of Fresh Patient Samples. 34th Annual Meeting & Pre-Conference Programs of the Society for Immunotherapy of Cancer (SITC 2019); Washington, D.C., USA. November 6 – 10, 2019. Journal for ImmunoTherapy of Cancer. 2019; 7 (Suppl 1): 282. DOI: 10.1186/s40425-019-0763-1